Pregnancy is a state of increasing insulin resistance that predisposes women to hyperglycemia. Maternal hyperglycemia results in fetal hyperinsulinemia and may predispose to excessive fetal growth. Identifying and properly managing gestational diabetes is important as it reduces risks of adverse pregnancy outcomes such as cesarean section, pre-eclampsia and shoulder dystocia.
Frequent glucose monitoring is critical to guiding therapy and occurs at least four times a day on a daily basis. Our own experience is to initiate therapy when at least 20% of recorded glucose values are above the target. A combination of rapid-acting and intermediate- or long-acting insulins is typically required to achieve euglycemia in women with frequent hyperglycemia.
Glyburide stimulates the maternal pancreas to increase insulin production and is effective at achieving euglycemia. Metformin increases insulin sensitivity and typically does not because significant hypoglycemia.
|
Recent studies demonstrate that metformin is a viable alternative to insulin for gestational diabetes mellitus management; however, there is a high failure rate requiring insulin supplementation.
Recent data demonstrate that identifying and managing gestational diabetes is an important part of prenatal care to maximize perinatal outcomes. The variety of therapies available to maintain euglycemia continues to expand and it is important for obstetrical care providers to keep abreast of new therapeutic opportunities.
Although injectable insulin has been available for decades, advances in insulin design have truly revolutionized how it is administered and, ultimately, improved glucose management.
Beyond insulin, oral hypoglycemic agents such as glyburide and metformin continue to gain popularity due to patients’ requests and ease of use. In this review, we present the available data to help providers understand what therapies are available, their unique strengths and weaknesses, and how to initiate and escalate doses to achieve maternal euglycemia.
More than ever before, providers must be familiar with the options for gestational diabetes mellitus (GDM) management. After decades of uncertainty, evidence confirming that treatment of GDM reduces adverse perinatal outcomes highlights the need to understand the strengths and weaknesses of the therapeutic options available for maintaining euglycemia.
The incidence of GDM continues to rise in the shadow of the obesity epidemic without any signs of easing. Alternative screening and diagnostic proposals could double or triple the prevalence over night, assuring that few medical providers would be exempt from managing large numbers of these women.
Physiology in Brief
To see how to oversee GDM, it is valuable to get comfortable with the physiological changes in glucose digestion that happens during pregnancy. Pregnancy is a condition of quickened starvation because of the expanded metabolic needs of both the embryo and mother.
Above all, ordinary pregnancy is portrayed by changes in the fringe tissue reaction towards insulin. Despite the fact that pregnancy starts with a condition of expanded insulin affectability during the principal trimester, the rest of the pregnancy is characteristically described by a prodiabetogenic state with decreased insulin affectability and compensatory hyperinsulinemia.
These progressions are generally clear as the pregnancy propels past the main trimester. In ladies with diabetes, there is a family member (GDM or diabetes mellitus (DM Type 2) or supreme insulin lack (DM Type 1) and paying little mind to the etiology, the accessible insulin is deficient to keep up euglycemia.
The net outcome is new-beginning hyperglycemia in the beforehand euglycemic mother (GDM) or more significant hyperglycemia requiring expanded exogenous insulin (DM Type 1 and2). Glucose, by means of encouraged dissemination, crosses the placenta to the fetus.
The approved Pedersen speculation joins maternal hyperglycemia with ensuing fetal hyperglycemia, which thusly animates fetal pancreatic B cells to emit insulin and IGFs. It is this fetal hyperinsulinemia that inclines the embryo to an anabolic state and prompts possible inordinate fetal development.
Rationale for therapy
It has for quite some time been realized that GDM is related with an assortment of unfriendly results, for example, fetal macrosomia, shoulder dystocia, birth injury, requirement for cesarean area and toxemia.
Just in the most recent decade have we started to collect top notch proof that distinguishing GDM and streamlining maternal glycemia with diet and pharmacotherapy improves maternal and fetal results? Despite the fact that the US Prevention Service Task Force have established that there are deficient information to help screening and treatment, an update has been drafted suggesting screening following 24 weeks.
Methodical surveys and meta-examinations have shown that screening and treatment of GDM diminishes the danger of results, for example, enormous for gestational age youngsters, shoulder dystocia (and assumed birth injury) and toxemia.
Management
Current administration of diabetes spins around building up ideal glycemic control. Glucose observing, way of life changes, consideration and adherence to a reasonable eating regimen, and pharmacotherapy when diet neglects to address hyperglycemia are exceptionally significant parts of the consideration plan.
Expanding insulin obstruction with progressing gestational age frequently brings about the requirement for pharmacotherapy in GDM ladies in order to diminish the recurrence of hyperglycemia.
Glucose monitoring
Self-checking of blood glucose ought to be led before breakfast and 1 or 2 h after breakfast, lunch and supper. The utilization of post rather than pre-prandial levels to manage treatment has been related with improved results, including lower hazard for macrosomia, neonatal hypoglycemia and lower cesarean conveyance for work dystocia.
Premeal glucose estimations might be included all the more testing cases. The ideal degree of glycemic control has not been set up. Persistent glucose observing has not been shown to improve results as of right now and bigger randomized preliminaries are in progress to decide the utility of glucose checking in GDM the executives.
The target of dietary treatment is, fundamentally, to control postprandial glucose levels and guarantee sufficient maternal–fetal nourishment. A normal weight lady will require 30–35 kcal/kg/day. Ladies who are underweight may require 30–40 kcal/kg/day, while the individuals who are overweight (>120% ideal body weight) may require less calories.
An eating routine high in starches (50–60%) has been thought to expand the danger for inordinate weight gain and postprandial hyperglycemia, and this has upheld the reasoning that maybe a lower extent of sugars would be more proper. Information has shown that a low glycemic list diet could be desirable over an unlimited eating regimen to limit insulin use.
Given the expected worry for creating maternal ketones with contrasting eating regimens, it is consoling that an orderly survey has not exhibited any hindering impacts from an assortment of varying weight control plans, including low glycemic and lower sugar (<45%) eats less carbs. Alternately, clear obstetrical advantages have not been exhibited with a specific eating routine.
That being stated, numerous focuses normally propose three unsurprising dinners for every day with two span bites to limit postprandial glucose outings. We likewise prescribe ladies to burn-through complex as opposed to basic sugars for a similar explanation.
Every day physical exercise diminishes insulin opposition. Albeit a randomized preliminary of 19 ladies exhibited improved fasting and postprandial qualities in ladies who practiced 20 min daily, three times each week, most investigations have indicated blended outcomes concerning the advantage of activity in GDM.
Right now, there is deficient information to exhibit noteworthy focal points to glycemic control; in spite of the fact that we accept that it is judicious to keep up normal exercise as a feature of a solid way of life for ladies with and without GDM.
Pharmacological Therapy
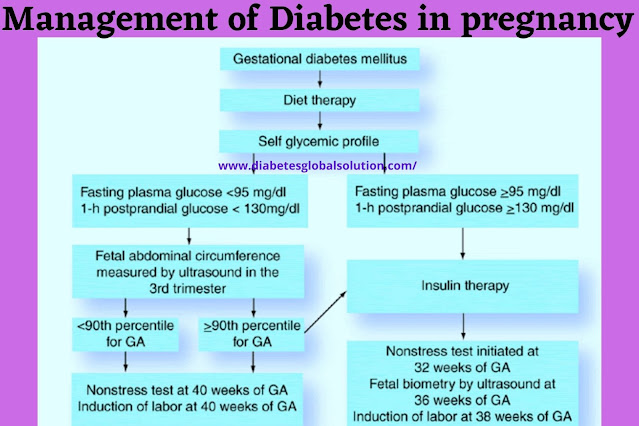
By and large, ladies with GDM may become euglycemic with diet alterations alone. However, 10–20% needs pharmacological help. Starting and upgrading treatment depends on fasting and postprandial glycemic control once a suitable eating routine is set up.
Danger factors for pharmacological help are like danger factors for clear Type 2 diabetes and incorporate BMI >30, early gestational age at finding and expanding glucose esteems on indicative testing.
Approved measures for diet disappointment don't exist and most experts utilize persevering raised fasting glucose levels of >95 mg/dl, 1 h postprandial >130–140 mg/dl or 2 h postprandial >120 mg/dl as signs for treatment.
Others have started treatment with as meager as two raised glucose esteems over a 2‑week period. The extent of qualities that must be over the objective so as to start treatment is obscure.
Our gathering regularly considers 20–half of qualities at some random time point as a sensible commencement point, and consider more forceful administration if fetal biometry on ultrasound proposes fetal hyperinsulinemia.
Apparently fourteen days of diet the board alone is a sensible beginning by and large, aside from when fasting esteems are more than 95 mg/dl, as this gathering unavoidably needs some pharmacological support.
Insulin
As of now, insulin remains the norm of care for glycemic control. Insulin is utilized to control hyperglycemia and keep up levels beneath suggested objectives. Insulin necessities increment all through growth.
Overall, insulin needs are 0.7–1.0 units/kg every day, given in isolated dosages. For GDM, we ordinarily partition insulin into prandial and basal insulin. Either fast acting (lispro or aspart) or short-acting (normal) prandial insulins are utilized to oversee glucose trips related with suppers.
Middle of the road acting insulin (nonpartisan protamine Hagedorn insulin [NPH]) or infrequently long-acting insulin (glargine/detemir) are utilized as basal insulin’s to smother maternal gluconeogenesis. As of late, lispro protamine (or unbiased protamine lispro) has opened up.
Insulin Dosing
Numerous ladies with mellow glucose journeys might be effectively made do with a basic evening time infusion of NPH at a portion of 0.2 units/kg of body weight. For more confounded cases, the absolute insulin prerequisite might be assessed by weight for ladies who require both insulin infusions to oversee fasting and postprandial glucose.
The best experience is with a blend of NPH and a fast/short-acting prandial insulin. Different regimens have been utilized, with no proof accessible that any are prevalent. A three-infusion routine is simple and generally utilized as a beginning stage. 66% of the absolute assessed portion is given before breakfast.
This is separated into 66% moderate acting anda third short-or quick acting insulin. The night portion is offered preceding supper and is 33% of the aggregate. NPH and short-/fast acting insulins are given in equivalent parts.
We follow glucose estimations for at any rate multi week before inception of insulin, recognizing which part of the day is related with steady hyperglycemic scenes. Insulins are started at a large portion of the determined weight-based portion and focused to cover times of hyperglycemia.
Insulins are expanded quickly to get euglycemia. In uncommon instances of outrageous maternal insulin opposition, we have utilized U-500 insulin to great impact; albeit more examinations are needed to offer more precise guidance.
Current contraindications include:
Ladies with a known unfavorable response to sulfonamides, sulfonylurea, carbonic anhydrase inhibitors, thiazides or circle diuretics ought not be recommended glyburide. For ladies who are not enduring oral taking care of, glyburide ought to be ended because of the danger for hypoglycemia.
Metformin is a biguanide that is utilized as a firstline oral operator outside of pregnancy for diabetes because of the usability and absence of huge results, aside from the uncommon entanglement of lactic acidosis.
It has been exhibited to cross the placental interface; despite the fact that, up to this point, has not been related with neonatal hypoglycemia. In contrast to insulin or glyburide, it lessens fringe insulin obstruction and doesn't have the regular concerning symptoms of insulin and glyburide, including weight gain and serious hypoglycemia.
Until now, metformin has not picked up a similar fame of utilization as glyburide in the USA as an elective oral hypoglycemic operator; albeit most obstetricians have some involvement in metformin during pregnancy because of the prevalence of utilization in ladies with polycystic ovarian disorder.
As of late, short-and some drawn out results concerning metformin introduction for GDM have opened up, which is significant data as metformin is known to cross the placenta to the fetal compartment in huge focuses.
Rowan et al. shown equality in a randomized preliminary among metformin and insulin for GDM; notwithstanding, over 40% of ladies randomized to metformin required some insulin supplementation. Glycemic control was comparable, as were maternal and neonatal results, however there was a high pace of metformin disappointment (46%) requiring supplemental insulin to accomplish euglycemia.
There was an unexplained increment in rashness, however this didn't show up clinically noteworthy. Favorable circumstances to metformin were noted, including diminished maternal weight gain just as expanded patient fulfillment.
The previous is especially significant for future wellbeing given the penchant for ladies with GDM to have weight concernsprior to pregnancy. In contrast to the involvement in glyburide, the posterity of the first randomized controlled preliminary is being followed-up following 2 and 5 years, with great neonatal information to guarantee no unforeseen long haul results to the posterity.
The primary assessment of the posterity at age 2 years showed negligible concerns. Albeit generally speaking fat was comparative in insulin and metformin gatherings, some particular biometric estimations (upper arm periphery and subscapular skin folds) were somewhat expanded in the metformin gathering and the clinical hugeness stays unsure.
Given the thorough assessments of metformin, we accept that metformin may locate a more conspicuous part in GDM the executives soon, maybe more so than glyburide. Presently, the adequacy and security of oral operators and injectable insulins are comparative.
In view of our own insight and audit of the writing, the impending dangers of oral hypoglycemic specialists show up indistinguishable to insulin and there are critical favorable circumstances for their remedy, including usability, understanding fulfillment, adherence and cost.
Be that as it may, there are circumstances where oral hypoglycemic operators are probably going to be improper, particularly as the maternal aggregate comes to take after people with pregestational diabetes to an ever increasing extent.
Questions remain concerning the drawn out security of oral hypoglycemic operators and these constraints ought to be surveyed with ladies when settling on insulin and an oral specialist.
Conclusion & Future Perspective
As the heftiness pandemic keeps on seething in the USA obviously we will think about more ladies with diabetes during pregnancy. In the course of the most recent decade, new choices have immediately opened up and there is each motivation to accept that this pattern will proceed.
Now and again, a portion of these alternatives have not been thoroughly tried for wellbeing before they picked up prominence and the ladies we care for will have progressively more choices to browse. It will get officeholder upon suppliers, with significantly more prominent thoroughness, to demand solid short-and long haul information to help their overseeing gestational diabetes: timing, choice and utilization of pharmacotherapy.
Tag
|



Post a Comment